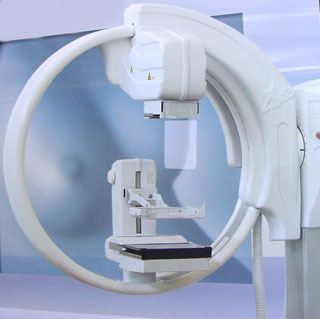
Digital Mammography
| |
 |
| |
|
- One of the most recent advances in x-ray mammography is digital mammography. Digital (computerized) mammography is similar to standard mammography in that x-rays are used to produce detailed images of the breast. Digital mammography uses essentially the same mammography system as conventional mammography, but the system is equipped with a digital receptor and a computer instead of a film cassette. Several studies have demonstrated that digital mammography is at least as accurate as standard mammography.
- Digital mammography allows faster and more accurate stereotactic biopsy so as "full-field" digital mammography system to screen for and diagnose breast cancer. With continued improvements, the "full-field" mammography systems may eventually replace traditional mammography.
- It is an X-ray examination done for early detection of breast diseases specially carcinoma. Examination is FDA approved and is superior in microcalcification detection
- Ductography examination, which is also available in our center, consists of contrast injection into a duct especially in cases of bleeding per nipple.
- Center also provide following services: breast biopsy, wire localization and cyst aspiration
How Does Digital Mammography Differ From Standard Mammography?
In standard mammography, images are recorded on film using an x-ray cassette. The film is viewed by the radiologist using a "light box" and then stored in a jacket in the facility’s archives. With digital mammography, the breast image is captured using a special electronic x-ray detector, which converts the image into a digital picture for review on a computer monitor. The digital mammogram is then stored on a computer. With digital mammography, the magnification, orientation, brightness, and contrast of the image may be altered after the exam is completed to help the radiologist more clearly see certain areas.
Data from German researchers suggest that the radiation dose can be reduced by up to 50% with digital mammography and still detect breast cancer as well as the standard radiation dose of film mammography. However, the radiation dose of standard film mammography is still extremely low and does not pose a risk to women.
From patient's perspective, a digital mammogram is the same as a standard film-based mammogram in that breast compression and radiation are necessary to create clear images of the breast. The time needed to position the patient is the same for each method. However, conventional film mammography requires several minutes to develop the film while digital mammography provides the image on the computer monitor in less than a minute after the exposure/data acquisition. Thus, digital mammography provides a shorter exam for the woman and may possibly allow mammography facilities to conduct more mammograms in a day. Digital mammography can also be manipulated to correct for under or over exposure after the exam is completed, eliminating the need for some women to undergo repeat mammograms before leaving the facility.
With digital mammography, the magnification, orientation, brightness, and contrast of the mammogram image may also be altered after the exam is completed to help the radiologist more clearly see certain areas of the breast.
So
In film mammography, which has been used for over 35 years, the image is created directly on a film. While standard film mammography is very good, it is less sensitive for women who have dense breasts. Prior studies have suggested that approximately 10 percent to 20 percent of breast cancers that were detected by breast self-examination or physical examination are not visible on film mammography. A major limitation of film mammography is the film itself. Once a film mammogram is obtained, it cannot be significantly altered; if the film is underexposed, for example, contrast is lost and cannot be regained.
Digital mammography takes an electronic image of the breast and stores it directly in a computer. Digital mammography uses less radiation than film mammography. Digital mammography allows improvement in image storage and transmission because images can be stored and sent electronically. Radiologists also can use software to help interpret digital mammograms. One of the obstacles to greater use of digital mammography is its cost, with digital systems currently costing approximately 1.5 to 4 times more than film systems.
Digital Mammography benefits include:
- Improved contrast between dense and non-dense breast tissue
- Faster image acquisition (less than a minute)
- Shorter exam time (approximately half that of film-based mammography)
- Easier image storage
- Physician manipulation of breast images for more accurate detection of breast cancer
- Ability to correct under or over-exposure of films without having to repeat mammograms
- Transmittal of images over phone lines or a network for remote consultation with other physicians
Digital mammography was significantly better in screening women who fit any of these three categories:
- under age 50 (no matter what level of breast tissue density they had)
- of any age with heterogeneously (very dense) or extremely dense breasts
- pre- or perimenopausal women of any age (defined as women who had a last menstrual period within 12 months of their mammograms)
There is no apparent benefit of digital over film mammography for women who fit ALL of the following three categories:
- over age 50
- those who do not have dense or heterogeneously (very dense) breast tissue
- those who are not still menstruating
NCI recommendation for screening mammograms (NCI: American National Cancer Institute)
NCI recommends that:
- Women in their 40s should be screened every one to two years with mammography
- Women aged 50 and older should be screened every one to two years
- Women who are at higher than average risk of breast cancer should seek expert medical advice about whether they should begin screening before age 40 and the frequency of screening
How does a postmenopausal woman over age 50 determine if she has extremely dense or heterogeneously dense breasts?
At present, this can only be determined by a prior mammogram. Usually the density rating on mammography should be noted in the written report from the interpreting radiologist who reads the mammogram. If it is not included in the mammography report, it can be determined by a radiologist or qualified mammography technologist by viewing a prior mammogram. Women who are uncertain about their density status should inquire about it at the time of their next mammography visit.
If a woman has dense breasts, will she have dense breasts for the rest of her life?
Breast density can change over time. Most frequently, breast tissue becomes less dense with age. Estrogen replacement therapy, menopause, and weight loss or gain can change a woman's breast density. If a woman has questions about her breast density, she can discuss it with her primary care physician or the staff at the clinic where she receives her mammograms.
Does getting a digital mammogram feel similar to getting a film mammogram?
From a woman's perspective, a digital mammography examination is similar to a traditional mammography examination. Positioning and compression of the breast are identical.
What other breast imaging techniques might be useful for breast cancer screening?
In addition to mammography, ultrasound and magnetic resonance imaging (MRI) are both sometimes used to screen for breast cancer. MRI has shown promise for women at high-risk for breast cancer.
Are there other possible advantages of digital mammography over film mammography?
Digital mammography offers other advantages over film, including improved ease of image access, transmission, retrieval and storage, and lower average radiation dose without a compromise in diagnostic accuracy. In addition, digital mammograms are less likely than film mammograms to be lost.
What levels of radiation are used for digital mammography vs. film mammography?
In DMIST, digital mammograms required approximately three quarters the radiation dose of film mammography. However, the dose in film mammography is quite low and poses no significant danger to patients.
What is telemammography?
Telemammography is the transmission of digital mammograms electronically so that they might be interpreted in a remote location. This can be accomplished through wireless networks (such as through satellites) or through more traditional wire-based networks. This may allow access to experts and second opinions more quickly for digital mammograms, particularly for women in underserved areas. Of course, second opinions are also available with film mammography by shipping mammograms using mail and other delivery services.
Why you should examine your breasts monthly?
Most breast cancers are first discovered by women themselves. When breast cancers are found early and treated promptly, they have excellent chances to be cured; learning how to examine your breasts properly can help save your life. Use the simple 3-step breast self-examination (BSE) procedure.
For the best time to examine your breasts (BSE: Breast Self Examination):
Follow the same procedure once a month about a week after your period, when breasts are usually not tender or swollen. After menopause, check breasts on the first day of each month. After hysterectomy, check your doctor or clinic for an appropriate time of the month.
Doing breast self-examination (BSE) will give you monthly peace of mind and seeing your doctor once a year will reassure you there is nothing wrong.
What you should do if you find a lump or thickening?
If a lump or dimple or discharge is discovered during BSE, it is important to see your doctor as soon as possible. Do not be frightened. Most breast lumps or changes are not cancer, but only your doctor can make the diagnosis.
How to examine your breasts?
1-In the shower:
Examine your breasts during bathing or showering. Hands glide easier over wet skin. Fingers flat move gently over every part of each breast. Use right hand to examine left breast, left hand for right breast. Check for any lump, hard knot or thickening.
2-In front of a mirror:
Inspect your breasts with arms at your sides. Next, raise your arms high overhead. Look for any changes in contour of each breast, a swelling, dimpling of skin or changes in the nipple. Then, rest palms on hips and press down firmly to flex muscles. Left and right breast will not exactly match - few women’s breasts do Regular inspection shows what is normal for you and will give you confidence in your examination.
3-Lying down:
To examine your right breast, put a pillow or folded towel under your right shoulder. Place right hand behind your head, this distributes breast tissue more evenly on the chest. With left hand, fingers flat, press gently in small circular motions around an imaginary clock face. Begin at outermost top of your right breast at 12 o'clock, and then move to 1 o'clock, and so on around the circle back to 12. A ridge of firm tissue in the lower curve of each breast is normal.
Then move an inch in, toward the nipple, keep circling to examine every part of your breast, including nipple. This requires at least three more circles. Now slowly repeat procedure on your left breast with a pillow under your left shoulder and left hand behind head.
Notice how your breast structure feels.
Finally, squeeze the nipple of each breast gently between thumb and index finger. Any discharge, clear or bloody, should be reported to your doctor immediately.
In case of pregnancy, the patient should inform us, so that we can contact her doctor previous to examination. |